Primary and community care
The tools developed for I-CARE & Share have been extensively tested across several Places and have a proven track record within general practice and community services.
Phase 1
Primary and community care was selected as phase 1 for the following reasons:
- General practice and community care manage the majority of palliative care patients.
- Care homes are situated in the community.
- 350 general practices are covered by just two IT systems, enabling quicker scale-up
- General practices have an obligation under the PCN DES to care plan care home patients. I-CARE & Share processes cover the NHS England requirements for this contractual obligation.
- There is an urgency to help patients wishing to stay at home to do so – especially given the pressures within the urgent and emergency care system.
- The wide variety of care plan types, quality and frequency across Cheshire and Merseyside warranted priority focus.
General practitioners and community care staff are highly trained in managing complex, frail and palliative care patients.
I-CARE & Share provides new tools to enable this to be more comprehensive and ensure their clinical care decisions influence other services appropriately.
Identification
- All practices should have a palliative care register with a minimum of 0.6% of the practice population.
- If the register is lower than this, consider using the EARLY tool (EMIS search) to identify patients who are likely to die in the next 6-12 months
Communication
- All initial Personalised Care Plans and DNACPR discussions should be conducted face to face with the patients and immediate carers or family. Using the Personalised Care Plan has been found to be a helpful framework.
Anticipatory Care Plan
- The Personalised Care Plan template covers this
Resuscitation Decision
- Discuss thoughts, feelings and decisions in regard to a cardiopulmonary resuscitation decision.
- If applicable, use the North West Unified Do Not Attempt Cardiopulmonary Resuscitation (uDNACPR) form.
- Problem code "Not for cardiopulmonary resuscitation" if this is the outcome for the patient
Escalation Plan
- The Personalised Care Plan template covers this
Share with other providers
- Save the Personalised Care Plan On the EMIS record
- Provide a printed copy to the patient/ carers
- Send a copy electronically to your GP OOH service
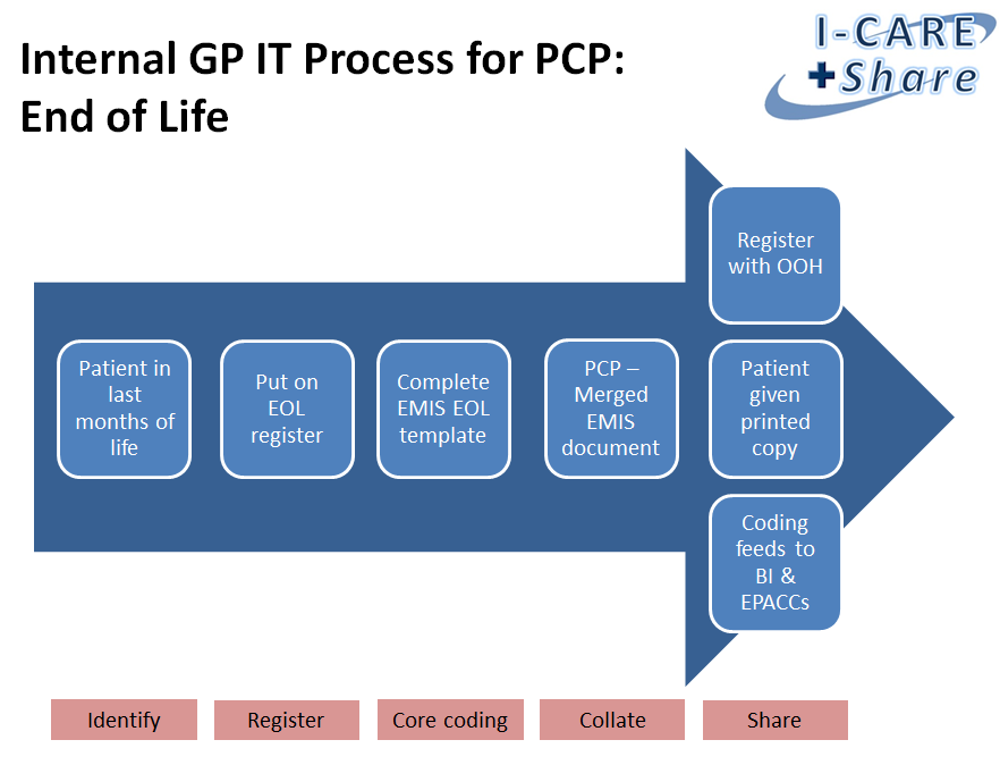
The process for a palliative patient is summarised below:
Frequently asked questions
Guides
Guides can be found on the I-CARE & Share resources page.
Useful links
Macmillan Advance Care Planning
What is Advance Care Planning?
EARLY Toolkit for Primary Care – using coding to identify patients at risk
Electronic Palliative Care Coordinating Systems (EPaCCS)
Ambitions for Palliative and End of Life Care: A national framework for local action 2021-2026
Network Contract Direct Enhanced Service Draft Outline Service Specifications (pages 22-28)